Hackensack Meridian Health Hackensack University Medical Center announced the implementation of a pilot program to screen cardiology patients for a common, yet often undiagnosed, sleep disorder. The Department of Sleep Medicine and the Heart and Vascular Hospital have successfully implemented a first of its kind collaborative clinical initiative to screen patients with cardiovascular disease, including Atrial Fibrillation (AFib) – a quivering or irregular heartbeat (arrhythmia) that can lead to blood clots, stroke, heart failure and other heart-related complications – for Obstructive Sleep Apnea, an involuntary cessation of breathing that occurs while a person is asleep. Using a state-of-the-art home sleep apnea test (HSAT) device called WatchPAT ™. The device tracks the patient’s heart rate, blood oxygen levels, air flow and breathing patterns while the patient is asleep in the comfort of their own home.
“Sleep apnea is very common in patients with Atrial Fibrillation, yet it’s not uniformly diagnosed, in part because it can be a major inconvenience and challenge for patients to stay overnight in a sleep lab at a medical facility,” said David Landers, M.D. vice chair, Heart and Vascular Hospital at Hackensack University Medical Center. “Sleep apnea is directly associated with cardiac disease. Getting treatment for this condition is key.”
The program, which began earlier this year, is being piloted at two cardiology offices. Patients are screened for risk factors, which include having a body mass index (BMI) over 35 and who have been told by a partner that they snore.
“Approximately 22 million adults suffer from sleep apnea, but what’s even more shocking is that 80 percent of these cases are undiagnosed,” said John Villa, D.O., medical director, Institute for Sleep/Wake Disorders at Hackensack University Medical Center. “Sleep apnea is associated with growing health problems including hypertension, cardiac arrhythmias, heart failure and stroke. It can also cause daytime sleepiness, depression, irregular sleep cycles and poor sleep quality.”
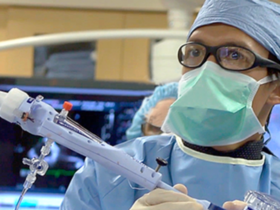
Those patients thought to be at high-risk for sleep apnea are given WatchPAT to conduct a sleep test at home. Sleep study data are collected during the test and automatically sent to CloudPAT™ Itamar’s secure server. Once the test is complete, a comprehensive report using WatchPAT’s True Sleep Time, Sleep Architecture and Central Plus algorithms is automatically generated and sent to the prescribing physician.
Pilar Ortiz, an advanced practice nurse (APN) in the Department of Sleep Medicine at Hackensack University Medical Center, screens patients for sleep apnea by asking a series of questions about the patient’s sleep experience, daytime sleepiness and physical characteristics, including weight. This screening tool identifies people who are likely to have sleep apnea or who potentially may develop it, so that once identified, they are given the WatchPAT to take home and become educated on how to use it.
“Patients in the pilot have been diagnosed with various forms of sleep apnea, from mild, to moderate and even severe sleep apnea,” says Pilar Ortiz, APN. “Educating our patients and their families about sleep apnea is crucial. Now that sleep apnea can be more easily detected, through a device patients can wear at home, we can more easily identify those most at risk to help them get the treatment they need.”
“This initiative is the result of innovation and collaboration on the part of our multidisciplinary, clinical teams,” said Mark D. Sparta, FACHE, president and chief hospital executive, Hackensack Meridian Health and executive vice president, Population Health, Hackensack Meridian Health. “I commend the Department of Sleep Medicine and the Heart and Vascular Hospital for their efforts to work together to improve the health and well-being of our patients.”
Once diagnosed, patients are sent to a primary care doctor or a sleep specialist to discuss available treatments. Three potential treatment options include wearing a CPAP, also known as continuous positive airway pressure, which uses mild air pressure to keep a patient’s breathing airway open; wearing an oral appliance to pull the airway forward; or surgery to the upper airway.
“Treating sleep apnea helps the management of the other medical conditions, including the metabolic or cardiac issues from which patients may suffer,” added. Dr. Villa. “Once a patient begins treatment, the side effects caused by sleep apnea begin to improve, including daytime sleepiness.”
“This innovative collaborative program is simultaneously and synergistically treating patients suffering from sleep apnea and cardiovascular disease,” said Michael Horton, administrative director, Clinical Services, Hackensack University Medical Center. “Through this program, we are raising the awareness of cardiac patients that sleep apnea is a common disorder that can be easily diagnosed and treated.”